Top 10 Cancer Prevention Habits Backed by Science
Cancer Prevention Series Part 1: Official Worldwide Guidelines
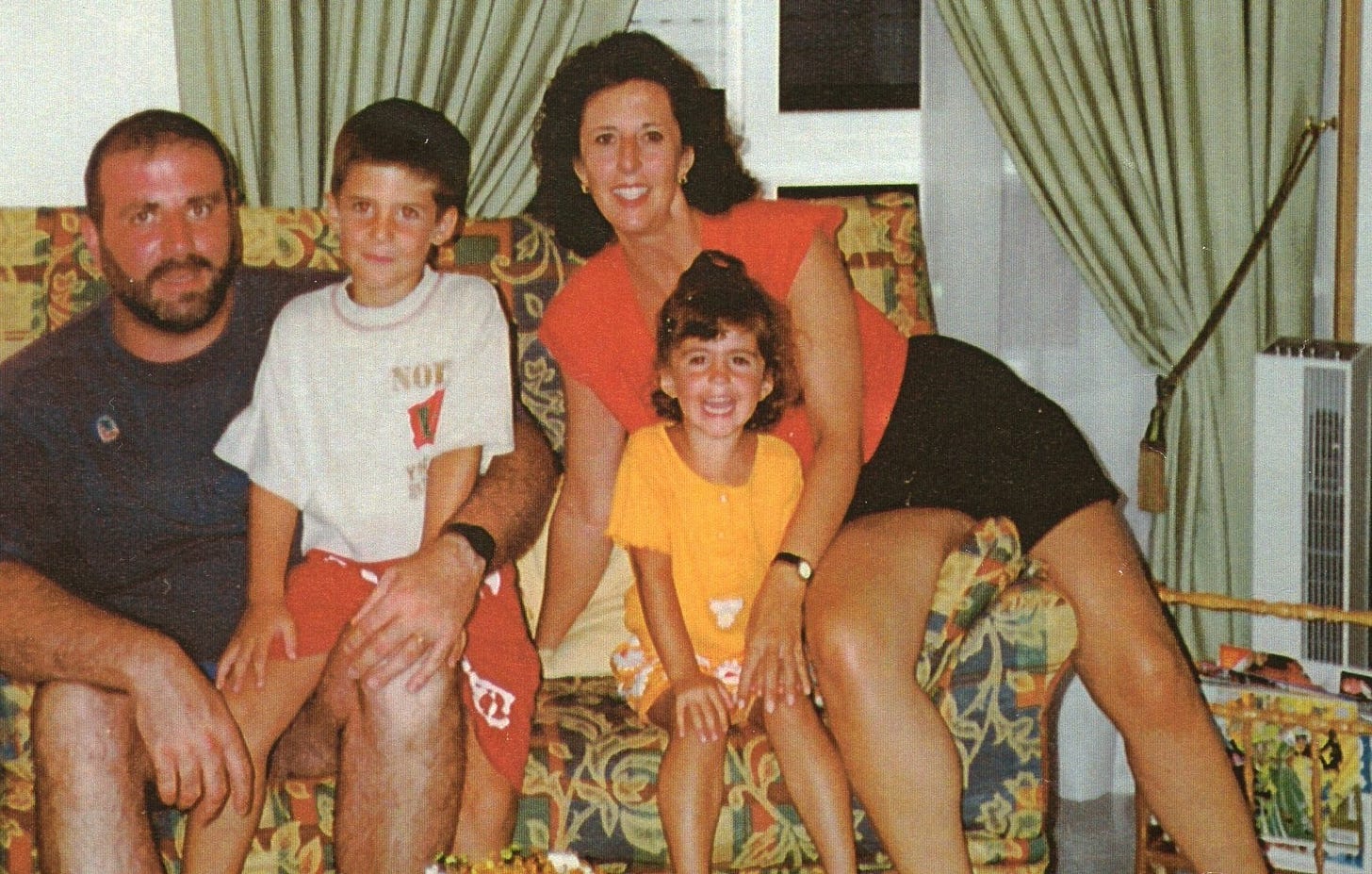
Christmas is a time for family, gifts, community, and gratitude.
When I think of those words, I think of my mother. I also think of you, and of every person who reads these emails hoping to live a longer, healthier life.
This year, in honor of my mom and as a heartfelt thank you to this community, I’m creating something I wish she — and we — had had earlier:
🎁 A completely free series on cancer prevention.
Why This Series Matters So Much
Cancer accounts for one in eight deaths worldwide.
After years of being the second leading cause of mortality, it has already become the number one cause of death in several regions, and by the end of this century, it is estimated to be the leading cause of death in all countries.
About 1 in 5 men and 1 in 6 women will develop cancer at some point in their lives, and 1 in 8 men and 1 in 11 women will die from it.
The most common types of cancer vary by gender:
In women: breast, lung, and colorectal cancer
In men: lung, prostate, and colorectal cancer
Here’s the part that changes everything:
More than 90% of cancers are attributed to modifiable risk factors such as smoking, being overweight, physical inactivity, alcohol consumption, and an inadequate diet.
Yet one of the most persistent myths about cancer is that “it’s mostly genetic.” While genes do play a role, for most people they explain only a small fraction of overall cancer risk.
The largest share comes from what we’re exposed to and what we do, day after day — the habits, environments, and choices we can gradually influence.
I wrote about some of the most common health myths debunked by science in this previous post, and I strongly encourage you to read it so you don’t waste time, money, or emotional energy on misinformation.
Confession time: I used to believe some of them too.
Today, I want to focus on what serious, evidence-based organizations actually agree on about prevention — and how you can start applying it in real life.
Why I’m Doing This
As a doctor, patient, and daughter, I have seen cancer from every angle.
My mother was diagnosed with lung cancer despite never having smoked. She underwent chemotherapy, but it was ineffective. She died one year later, while I was in medical school.
Around that time, I learned about another doctor with metastatic ovarian cancer, whose prognosis was similarly poor. But alongside her oncology treatment, she embraced an integrative approach — exercise, nutrition, psychological support, and complementary therapies. Not only did she recover, but she later had children.
It shook me.
Why did my mother never receive this kind of integrative support?
Why was the system almost entirely focused on treating disease, and so little on preventing it and supporting the whole person?
Later, I struggled too — with depression, insomnia, and anxiety — and again, the only solution offered was an antidepressant. No therapy, no support, just a prescription.
These experiences are the reason I do what I do.
They’re the reason I built Zenith Within. From the bottom of my heart, I truly hope this series helps you protect yourself and the people you love.
Today’s Focus: What All the Major Guidelines Agree On
There is a lot of noise online about cancer: miracle diets, detoxes, superfoods, and extreme fear.
But when we zoom out and ask:
“What do the major scientific and medical organizations say about cancer prevention?”
we get a very clear, reassuring answer.
Three big players have independently reviewed the evidence:
World Cancer Research Fund / American Institute for Cancer Research (WCRF/AICR)
American Cancer Society (ACS)
European Code Against Cancer (ECAC)
And despite different methods and regions, they all converge on the same core habits.
Even more encouraging:
People with greater adherence to the WCRF/AICR cancer prevention recommendations have about a 27% lower overall risk of developing cancer.
If that effect came in pill form, it would dominate headlines. Don’t you think?
But our healthcare system makes far more money treating disease than preventing it. The sicker you are, the more profitable you become.
Think of your daily choices as bricks. One brick doesn’t build a house. But brick by brick, you build a structure strong enough to protect you in a storm.
Today, I’ll show you the unified core of these three guidelines — a simple map of where prevention efforts matter most. In future emails, we’ll go deeper into different areas.
The 10 Core Habits of Cancer Prevention
What WCRF/AICR, ACS, and the European Code all align on.
1. Don’t smoke — and avoid secondhand smoke
Tobacco, in any form, is packed with carcinogens and is still the single most important preventable cause of cancer.
If you smoke, quitting is the most powerful cancer-prevention step you can take — for yourself and everyone who loves you. If you don’t smoke, protect that win by avoiding secondhand smoke at home, at work, and in social spaces whenever possible.
Nicotine is highly addictive. You deserve support, not blame.
2. Maintain a healthy body weight (especially around the waist)
Excess body fat, particularly around the abdomen, is linked to a higher risk of several cancers, including colorectal, breast (postmenopausal), endometrial, pancreatic, kidney, and others.
The goal isn’t a “perfect body”; it’s less chronic inflammation, more metabolic balance.
Key ideas the guidelines agree on:
Try to keep your weight within a healthy range throughout adulthood.
Pay attention to waist circumference, not just the scale — abdominal fat is especially risky.
Small, steady improvements matter more than extreme short-term changes.
Think of it as gently steering the ship a few degrees in a healthier direction — and keeping it there.
3. Move more, sit less
Physical activity does much more than burn calories. It sends a powerful signal to your cells about how they should function, divide, and repair.
The guidelines recommend:
Adults:
At least 150–300 minutes per week of moderate-intensity activity (like brisk walking), or
75–150 minutes per week of vigorous activity (like running), or a mix.
Children and adolescents:
At least 60 minutes per day of moderate to vigorous activity.
Everyone:
Reduce and break up long periods of sitting (TV, computer, scrolling on your phone).
The best workout is the one you’ll actually repeat. Whether that’s the gym, a home routine, or a daily walk—your body benefits from all of it: walking, dancing, stretching, lifting, biking, gardening, stairs.
4. Build a mostly plant-based, high-fiber plate
All three guidelines emphasize a similar pattern:
More of:
Vegetables (especially non-starchy ones)
Fruits
Whole grains
Legumes (beans, lentils, chickpeas, peas)
Less of:
Refined grains and ultra-processed foods
Foods and drinks high in added sugars
Foods high in unhealthy fats and salt
A plant-rich, high-fiber pattern:
Helps prevent weight gain, overweight, and obesity
Supports gut health, which is closely linked to immunity and inflammation
Reduces the risk of colorectal cancer, among others
You don’t have to be vegan to benefit. Just start shifting the center of your plate towards plants.
5. Limit red meat and keep processed meat as low as possible
The evidence is consistent: high intakes of red and processed meat increase the risk of colorectal cancer.
The guidelines suggest:
If you eat red meat (beef, pork, lamb), keep it to no more than ~350–500 g (12–18 oz) cooked per week.
Aim for very little, if any processed meat (bacon, ham, sausages, hot dogs, deli meats).
Fish, poultry, eggs, and plant proteins are excellent alternatives, and you can still meet your protein and nutrient needs without relying on red or processed meat.
This isn’t about never touching a burger again. It’s about making red and processed meat the exception, not the default.
6. Avoid sugary drinks and limit ultra-processed foods
Sugar-sweetened drinks are strongly linked to weight gain, overweight, and obesity, which in turn raise the risk of many types of cancer.
The shared recommendations:
Avoid or minimize sugar-sweetened beverages (sodas, energy drinks, sweetened teas, many fruit drinks).
Prefer water, unsweetened tea, or coffee without added sugar.
Limit fruit juice, even 100% juice — it can act more like a sugary drink than whole fruit.
Reduce fast food and ultra-processed products high in sugar, refined starches, and unhealthy fats.
A simple starting point:
Swap one sugary drink per day for water or unsweetened tea.
That single habit, repeated daily, can make a huge difference over the years.
7. If you drink alcohol, less is better — none is best
Alcohol (and its metabolite acetaldehyde) is classified as a Group 1 carcinogen, meaning it can cause cancer in humans.
It increases the risk of several cancers, including breast, colorectal, esophageal, and liver cancer — even at low to moderate levels.
The guidelines are very clear:
For cancer prevention, not drinking alcohol is the safest choice.
If you do drink, staying within low-risk national guidelines is better than exceeding them — but from a cancer perspective, less is always better.
8. Don’t rely on supplements for cancer prevention
High-dose supplements have not consistently shown the protective effects that observational studies suggested, and in some cases (like high-dose beta-carotene in smokers), they have increased cancer risk.
The guidelines agree:
Do not use high-dose dietary supplements for cancer prevention.
Aim to meet nutrient needs through a varied, whole-food diet.
Use supplements only when medically indicated (e.g., deficiencies, pregnancy), guided by a qualified professional.
Food behaves in the body differently than isolated, concentrated nutrients.
Nature designed nutrients to travel with fiber, water, and thousands of other compounds — not alone in a capsule.
9. Protect your skin and reduce harmful environmental exposures
UV radiation from the sun and tanning beds increases the risk of skin cancer.
Key messages:
Avoid excessive sun exposure, especially around midday.
Use a broad-spectrum sunscreen (SPF 30+) and apply enough, reapplying every 2 hours and after swimming/sweating.
Avoid tanning beds entirely.
Beyond UV, we are also exposed to environmental and occupational carcinogens (chemicals, dust, fibers, certain metals) that can increase cancer risk.
Whenever possible:
Follow safety guidelines at work.
Stay informed about local risks (like radon) and test your home where recommended.
Support public health policies that reduce environmental pollutants.
However, up to 95% of the United States population has a vitamin D deficiency, with levels even higher in many European countries.
Worried about vitamin D deficiency?
You can reach optimal levels without the risk of cancer skin. If vitamin D supplementation is indicated in your case, it would be ideal to combine it with vitamin K2 to:
Increase bone mineral density
Reduce the risk of coronary artery disease
10. Use modern medicine for prevention: vaccines, screening, and (for women) breastfeeding choices
Prevention also includes vaccines and early detection.
The guidelines recommend:
Vaccination against:
Hepatitis B (for newborns and at-risk adults)
Human papillomavirus (HPV) (for girls and, in many countries, boys)
Participation in organized screening programs for:
Colorectal cancer (men and women)
Breast cancer (women)
Cervical cancer (women)
For women:
Breastfeeding, when possible, reduces the mother’s risk of breast cancer and helps lower the child’s risk of excess weight gain.
Menopausal hormone therapy can be very helpful for some women, but it should be used thoughtfully and individually, as it can increase the risk of certain cancers.
For cancer survivors:
When medically appropriate, following these lifestyle principles (healthy weight, plant-rich diet, physical activity, limited alcohol, no smoking) can improve quality of life and may support better outcomes.
Supplements specifically for “cancer survival” are not supported by strong evidence, unless prescribed for other reasons.
Where to Start This Week
This is a lot of information. I don’t want you to feel overwhelmed; I want you to feel empowered.
So this week, choose just one of these:
Swap one sugary drink for water or unsweetened tea.
Add one extra serving of vegetables to your main meal.
Take a 10–15 minute walk after a meal instead of scrolling on your phone.
That’s it. No perfection. No guilt. Just one small vote for your future self.
You don’t have to change everything to change something.
And “something”, repeated over time, changes everything.
What’s Coming Next in This Free Series
In the upcoming emails, we’ll zoom into specific topics.
If you’d like to read about something in particular, feel free to let me know in the comments. I always love talking with you!
From My Heart to Yours 💛
If cancer has touched your life — your own diagnosis, a parent, partner, child, sibling, or friend — I see you. You are not alone here.
This series is dedicated to my mother… and to you, and to every person you love.
If today’s post was helpful, it would mean a lot if you:
Hit “like” or ❤️
Or share it with someone who could benefit
Or reply and tell me: Which habit feels most realistic for you to work on this month?
To your zenith within,
Sara Redondo, MD, MS
References:
International Agency for Research on Cancer. Global Cancer Observatory: Cancer Today [internet]. 2022. Available from: https://gco.iarc.fr/today/en.
GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016 Oct 8;388(10053):1459-1544. doi: 10.1016/S0140-6736(16)31012-1.
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018 Nov 10;392(10159):1736-88. doi: 10.1016/S0140-6736(18)32203-7.
Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016 Nov 7;37(42):3232-3245. doi: 10.1093/eurheartj/ehw334.
Canadian Cancer Statistics Advisory Committee, Canadian Cancer Society, Statistics Canada, Public Health Agency of Canada. Canadian Cancer Statistics 2021 [internet]. 2021. Available from: https://cancer.ca/Canadian-Cancer-Statistics-2021-EN.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018 Nov;68(6):394-424. doi: 10.3322/caac.21492.
International Agency for Research on Cancer. Global Cancer Observatory: Cancer Today [internet]. 2022. Available from: https://gco.iarc.who.int/media/globocan/factsheets/populations/900-world-fact-sheet.pdf.
Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018 Jan;68(1):31-54. doi: 10.3322/caac.21440.
Brown KF, Rumgay H, Dunlop C, Ryan M, Quartly F, Cox A, et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br J Cancer. 2018 Apr;118(8):1130-1141. doi: 10.1038/s41416-018-0029-6.
Asociación Española Contra el Cáncer. Prevención del cáncer [internet]. Available from: https://www.aecc.es/es/todo-sobre-cancer/prevencion.
Clinton SK, Giovannucci EL, Hursting SD. The World Cancer Research Fund/American Institute for Cancer Research Third Expert Report on Diet, Nutrition, Physical Activity, and Cancer: impact and future directions. J Nutr. 2020 Apr 1;150(4):663-671. doi: 10.1093/jn/ nxz268.
U.S. Food & Drug Administration. Spilling the beans: how much caffeine is too much? [internet]. 2024 Aug 28. Available from: https://www.fda.gov/consumers/consumer-updates/spilling-beans-how-much-caffeine-too-much.
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies). Scientific opinion on the safety of caffeine. EFSA J. 2015;13(5):4102, 120 pp. doi: 10.2903/j.efsa.2015.4102.
Wikoff D, Welsh BT, Henderson R, Brorby GP, Britt J, Myers E, et al. Systematic review of the potential adverse effects of caffeine consumption in healthy adults, pregnant women, adolescents, and children. Food Chem Toxicol. 2017 Nov;109(Pt 1):585-648. doi: 10.1016/j.fct.2017.04.002.
Malcomson FC, Wiggins C, Parra-Soto S, Ho FK, Celis-Morales C, Sharp L, Mathers JC. Adherence to the 2018 World Cancer Research Fund/American Institute for Cancer Research cancer prevention recommendations and cancer risk: a systematic review and meta-analysis. Cancer. 2023 Sep 1;129(17):2655-2670. doi: 10.1002/cncr.34842.
Rock CL, Thomson C, Gansler T, Gapstur SM, McCullough ML, Patel AV, et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA Cancer J Clin. 2020 Jul;70(4):245-271. doi: 10.3322/caac.21591.
Schüz J, Espina C, Villain P, Herrero R, Leon ME, Minozzi S, et al. European Code against Cancer 4th Edition: 12 ways to reduce your cancer risk. Cancer Epidemiol. 2015 Dec;39 Suppl 1. doi: 10.1016/j.canep.2015.05.009.
Leon ME, Peruga A, McNeill A, Kralikova E, Guha N, Minozzi S, et al. European Code against Cancer, 4th Edition: Tobacco and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S20-33. doi: 10.1016/j.canep.2015.06.001.
Anderson AS, Key TJ, Norat T, Scoccianti C, Cecchini M, Berrino F, et al. European Code against Cancer 4th Edition: Obesity, body fatness and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S34-45. doi: 10.1016/j.canep.2015.01.017.
Leitzmann M, Powers H, Anderson AS, Scoccianti C, Berrino F, Boutron-Ruault MC, et al. European Code against Cancer 4th Edition: Physical activity and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S46-55. doi: 10.1016/j.canep.2015.03.009.
Norat T, Scoccianti C, Boutron-Ruault MC, Anderson A, Berrino F, Cecchini M, et al. European Code against Cancer 4th Edition: Diet and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S56-66. doi: 10.1016/j.canep.2014.12.016.
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Personal habits and indoor combustions. Volume 100 E: A review of human carcinogens. Lyon: International Agency for Research on Cancer; 2012.
Schütze M, Boeing H, Pischon T, Rehm J, Kehoe T, Gmel G, et al. Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ. 2011;342:d1584.
Scoccianti C, Cecchini M, Anderson AS, Berrino F, Boutron-Ruault MC, Espina C, et al. European Code against Cancer 4th Edition: Alcohol drinking and cancer. Cancer Epidemiol. 2016 Dec;45:181-8. doi: 10.1016/j.canep.2016.09.011.
McColl N, Auvinen A, Kesminiene A, Espina C, Erdmann F, de Vries E, et al. European Code against Cancer 4th Edition: Ionising and non-ionising radiation and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S93-100. doi: 10.1016/j.canep.2015.03.016.
Espina C, Straif K, Friis S, Kogevinas M, Saracci R, Vainio H, et al. European Code against Cancer 4th Edition: Environment, occupation and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S84-92. doi: 10.1016/j.canep.2015.03.017.
McColl N, Auvinen A, Kesminiene A, Espina C, Erdmann F, de Vries E, et al. European Code against Cancer 4th Edition: Ionising and non-ionising radiation and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S93-100. doi: 10.1016/j.canep.2015.03.016.
Scoccianti C, Key TJ, Anderson AS, Armaroli P, Berrino F, Cecchini M, et al. European Code against Cancer 4th Edition: Breastfeeding and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S101-6. doi: 10.1016/j.canep.2014.12.007.
Friis S, Kesminiene A, Espina C, Auvinen A, Straif K, Schüz J. European Code against Cancer 4th Edition: Medical exposures, including hormone therapy, and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S107-19. doi: 10.1016/j.canep.2015.08.003.
Villain P, Gonzalez P, Almonte M, Franceschi S, Dillner J, Anttila A, et al. European Code against Cancer 4th Edition: Infections and cancer. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S120-38. doi: 10.1016/j.canep.2015.10.006.
Armaroli P, Villain P, Suonio E, Almonte M, Anttila A, Atkin WS, et al. European Code against Cancer, 4th Edition: Cancer screening. Cancer Epidemiol. 2015 Dec;39 Suppl 1:S139-52. doi: 10.1016/j.canep.2015.10.021.
Linus Pauling Institute, Oregon State University. Micronutrient inadequacies in the US population: an overview [internet]. 2018 Mar. Available from: https://lpi.oregonstate.edu/mic/micronutrient-inadequacies/overview.
Biesalski Hans K, Jana T. Micronutrients in the life cycle: Requirements and sufficient supply. NFS J. 2018 June 1;11:1–11.





HepB vaccine for newborns? I can’t take you seriously.
Thank you Dr. Sara, I am currently going through diagnosis and just had my life saved at the hospital. As a Reiki Master Teacher and life long health food enthusiast I see how stress and environment are equally as important, if not more so, than proper diet and lifestyle habits. I have a strong Spiritual practice, so good, in fact, that I was able to sustain an unhealthy situation for far too long. And now my healing journey really begins...I am back with my grown children in a safe and clean environment, feeling supported and loved...Meat, mostly chicken and turkey is encouraged in my situation as I need protein and iron. Thank you for this series, it is arriving in perfect Divine Right Timing.
With Blessings,
Star Bear Medicine Woman
🌹🙏🦢